A 13 year old girl with anemia and mucosal hyperpigmentation
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs". This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome.
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
A 13 year old female, presented with the chief complaints of :
- Fever since three days
- Abdominal pain since three days
- Blackish stools since three days
History of presenting illness:
Patient was apparently alright 3 days ago, then she developed fever, low grade, insidious in onset, intermittent associated with chills
Not associated with headache, nausea, weakness, body aches, dizziness
Vomitings 2 episodes - non bilious, non blood stained, non foul smelling, food as content
Cold since 3 days associated with nasal discharge
Cough since 3 days , moderate , non productive
Abdominal pain since 3 days , diffuse in nature, dull aching, non radiating, on and off, no aggravating or relieving factors.
Not associated with abdominal distension, constipation, diarrhoea
Altered bowel habits +
Increased stool frequency to 3times a day
Stools - blackish, minimal quantity, associated with straining during passage, foul smelling, non blood stained
Not associated with worms in stools, excessive mucoid discharge
No h/o trauma to abdomen, no h/o previous blood transfusions.
Daily routine of the patient -
She wakes up at 8 am in the morning, has rice with curry with a glass of tea, goes to school, has lunch provided in school- rice,curry and sambar daily, gets back to home, dinner at 7 pm , rice and curry and sleeps at around 10 pm.
Consumption of fruits, nuts, and dairy products are lacking in patient's diet.
Personal history
Diet - mixed
Appetite - decreased
Sleep - adequate
Bowel and bladder - blackish stools with increased frequency
No addictions
Birth and developmental history
Born via normal vaginal delivery to a healthy mother, no h/o nicu admissions, attained all developmental milestones at the right age
Birth weight - 2.5 kg
Family history
Parents- Consanguineous marriage+
Third degree consanguinity
No h/o short stature in family, constitutional delay
No h/o developmental delays, short stature in siblings (elder brother and younger sister)
No h/o genetic disorders running in the family
No h/o thyroid disorders
Hair - normal
Knuckle hyperpigmented?
Nails - normal
Tanners staging
Breast appearance - stage 1 (prepubertal)
Pubic hair - stage 1 (prepubertal)
Axillary hair - absent
Systemic examination-
GIT examination-
Inspection-
Shape of abdomen- scaphoid
No scars sinuses visible pulsations visible swellings, dilated veins abdominal distension.
All quadrants moving with respiration
Umbilicus inverted
On palpation-
No local rise of temperature
Tenderness present - diffuse
More in right hypochondrium, right iliac fossa, hypogastrium.
Abdomen - soft , mild splenomegaly.?
No guarding, rigidity
On Percussion-
Tympanic note +
On auscultation-
Bowel sounds heard
CVS
Inspection-
Shape of chest- elliptical
No scars dilated veins
No raised JVP
Palpation-
Apex beat felt in left 5th ICS MCL
No thrills, parasternal heave felt
On auscultation-
S1 S2 heard, no murmurs
Respiratory system examination-
Shape of chest elliptical
B/l symmetrical expansion of chest wall+
Position of trachea- central
Resonance present in all lung fields
BAE+ NVBS+
CNS examination
Higher mental functions- intact
Cranial nerves intact
Sensory- fine touch, crude touch, pressure, temperature, vibration senses intact.
Motor system
Power: 5/5 in both UL and LL
Bulk - normal
Tone- normal
Reflexes:
Biceps, Triceps Supinator Knee reflexes intact (++)
Ankle reflex 5+
No cerebellar signs noticed
Investigations -
Hemogram on 04/02/2024-
CUE- normal
Stool for occult blood- positive
Serology
Hbsag - negative
HIV - negative
HCV - negative
Widal test - negative
Dengue profile-
NS1 Ag- negative
IgM positive
IgG- negative
ECG -
LFT
TB - 1.54
DB - 0.54
ALT- 48
AST- 50
ALP - 224
TP- 6.4
A/G- 1.70
RFT
Urea - 27
Creatinine - 0.6
Uric acid - 2.2
USG abdomen-
Mild splenomegaly.
Few prominent mesenteric lymph nodes.
Chest x ray -
Provisional diagnosis-
?Dengue ( IgM positive - day 5 of illness)
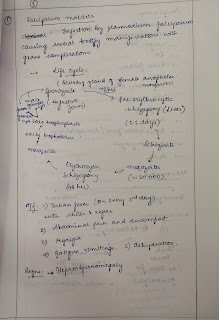
? Malaria (Tropical splenomegaly)
Anemia , thrombocytopenia under evaluation
Treatment given-
1. Tab. PCM 500mg PO SOS
2. Albendazole 400mg PO STAT
3. T. MVT PO OD






















Comments
Post a Comment